The Early Impacts of COVID-19 on Medical Trainees
/By Aishwarya Kumar
By now, there’s probably not a person in the world that hasn’t heard of the COVID-19 pandemic. My mother, who had never before expressed any interest in medical terminology, now gives me daily updates on virus transmission mechanisms and vaccine development. News broadcasts are inundated with constantly updated information about the increasing death toll and continuing debate on the supposed “human rights violations” of mandatory mask wearing. Suffice it to say, the pandemic has undoubtedly affected the lives of people all around the world since its first appearance in December 2019. We are in what sometimes seems like a never-ending quarantine, facing stressors such as loneliness, uncertainty, anxiety, and depression every single day. Many activities that were once easy, such as going for a workout at the gym or grabbing a quick coffee with friends, are now either impossible or difficult to partake in. The cultural landscape of education, work, and social interaction has changed drastically and will likely remain this way for an undetermined period of time.
As health care professionals, many of us have likely experienced the direct consequences of the virus to a closer degree than most. Since I was a first year medical student when the virus began its global spread, I underwent a period of uncertainty before state mandates were put into place. Would we be sent home to finish off the rest of the semester online? Would we still be able to finish our degrees on schedule if we could not follow accreditation guidelines? How am I supposed to know any anatomy without dissecting a cadaver? As a strong non-class-goer, I wasn’t as worried about these changes as I was about living near the (at the time) epicenter of the virus in New Jersey. Though my classmates and I ended up having to adjust to an online medical curriculum and all the glitches that came with it, it seemed like the first years were relatively the least affected. Second years had to deal with multiple scheduling changes to their USMLE Step 1, facing the threat of their exam being canceled even after arrival to the testing center the morning of. Third years were faced with cancelled audition rotations and online clinical rotations, an accommodation that might affect their residency applications as well as their skills as future physicians respectively. Fourth years in certain schools around the country were given early graduations and sent headfirst into frontline COVID-19 efforts in hospitals that were heavily affected by the virus. Stories surfaced about residents being forced to work with COVID-19 infected patients without proper personal protective equipment (PPE) and being encouraged to keep silent about these conditions. All of these things were piled on top of our already close proximity to patient deaths as well as personal ones.
To call all of this stressful and messy would be an understatement. Naturally, stress and uncertainty often lead to negative emotions. In times like these, where negativity is at an all-time high and it sometimes feels like terrible things are happening all around the world every day, it is not surprising that individual mental health may be at risk of taking a nose-dive. BereaveMed’s ultimate goal is to provide mental health resources and support to medical trainees. Additionally, grief can take many forms and does not just need to accompany loss of human life. In addition to grieving the loss of our patients and family members to this pandemic, we may also be grieving the loss of our former lives. We sent out surveys to our readers in order to see how they were affected by the pandemic. With this project, we hoped to provide medical trainees with an outlet to express their experiences with COVID-19. We hope that the results gathered from this survey can shine some light on what students and residents around the country are currently going through.
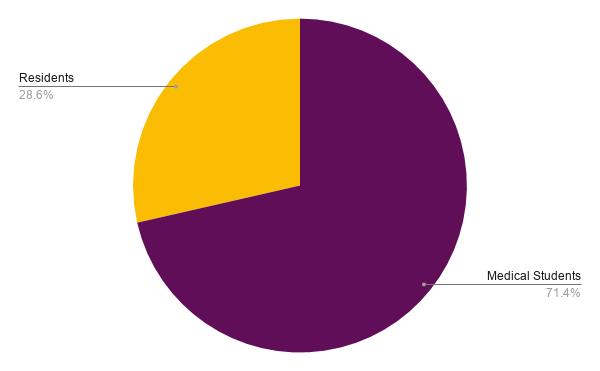
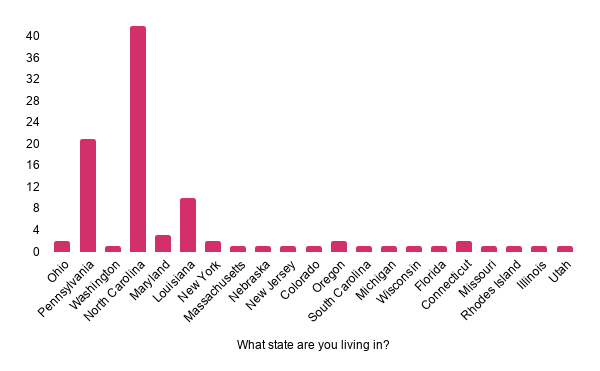
In total, we received 101 responses from both medical students and residents, the majority of whom were located in the Northeast.
In our survey, we asked individuals to describe their feelings regarding the pandemic in one word. Understandably, we noticed that a majority of participants were experiencing negative emotions. We constructed a world cloud that highlights some of the major sentiments expressed. Feeling anxious, uncertain, overwhelmed, exhausted, helpless, nervous, worried, and unsettled emerged as common and overlapping emotions between individuals.
We also examined common themes within trainees’ situations, coping mechanisms, and life changes as a result of the pandemic. Many individuals were:
in quarantine,
transitioning to online classes,
going home,
studying,
participating in research,
engaging in hobbies,
experiencing anxiety, and
communicating through technology.
Other themes that emerged were concerns regarding career-related situations. Trainees who had duties in clinical environments expressed that they were pulled from wards and lacked proper PPE. Recent fourth year graduates communicated that their match day and their medical school graduation were cancelled, while second year medical students spoke about how the pandemic interfered with their Step 1 exams. Residents reported that they were on-call and now had to partake in telemedicine. Many participants expressed difficulty in focusing and staying productive. Other worries included:
trouble with grocery shopping,
concern over the well-being of family members/themselves,
difficulty parenting, and
separation from their significant others.
Some individuals spoke about coping strategies citing mediation, religion, streaming, and exercise as activities they had become involved in since the start of the pandemic.
As of April 16, 2020, nearly two-thirds of the respondents knew someone that had contracted COVID-19. The graph below displays the responses we received to our question, “Have you lost anyone to this pandemic?” Although fewer participants had actually lost someone to the virus, these numbers have likely changed in the past five months, as the pandemic is still causing deaths in the United States.
It is clear that this pandemic has affected all of us deeply in a large number of ways. Although some individuals do admit to coping well and feeling relaxed, many of us feel the anxiety and fear that is currently plaguing countries and communities around the globe.
Now delving into some recently released literature regarding COVID-19, we found that patients are not the only ones who are succumbing to the virus. Studies have shown physician and health care provider deaths are on the rise as well. Two hundred seventy-eight physicians have died from the virus worldwide, ranging equally from a number of specialties. PPE shortages were a common cause of these deaths.1 Those of us entering the workforce may face anxiety regarding personal risk as well as the reliability and accessibility of the protective equipment that is given to us. A second study detailed the increasing number of suicides across the globe due to anxiety over the contagion and fear of social isolation. Individuals with pre-existing psychiatric conditions and others in vulnerable populations are especially at risk for experiencing negative moods due to the pandemic.2 Social and physical support is also lacking due to the social distancing measures in place. Physicians working with COVID-19 patients often find other housing to try and keep their families safe. Patients in hospitals often cannot receive visits from their families, regardless of the severity of their illness. Large funeral practices need to be completely revamped. How are we supposed to cope with the effects of this pandemic when these measures leave us with a much smaller support system? It is even difficult to practice common grieving practices amongst the comfort of family and friends. We have lost access to this support when we need it the most.
Unfortunately, I don’t think that there’s an easy fix to any of these issues. It is becoming increasingly important to follow proper protocols in regards to mask-wearing, quarantining, and maintaining physical distance from individuals not directly living in our homes. Especially in the United States, where it seems like the pandemic is never-ending, we must do our part in maintaining these precautions, lowering the curve, and protecting those who are more vulnerable to the devastating and unclear effects of the virus.
In truth, we cannot say for sure when things will go back normal. It is precisely for this reason that we must learn how to engage in self-care, be active about our mental health, and be there for each other more than ever. Personally, I have found a lot of solace in meditating five times a week, setting weekly goals for myself, frequently FaceTiming my family and friends, and learning makeup application from gurus on Youtube! Although it seems small, these are the things that help me stay sane when I hear sad news about our Thanksgiving break being canceled or not being able to physically participate in our OB/GYN simulation labs. It isn’t a perfect system, and though I do sometimes find myself frustrated and anxious about our situation, it’s important that we try our best!
In this same vein, we asked our survey participants to offer some words of encouragement and advice to their fellow medical trainees. It is our hope that in hearing what they have to say, we can all feel less alone and stand in solidarity during these trying times.
References
Ing EB, Xu QA, Salimi A, Torun N. Physician deaths from coronavirus (COVID-19) disease. Occup Med (Lond). 2020;70(5):370-374. doi:10.1093/occmed/kqaa088
Sher L. The impact of the COVID-19 pandemic on suicide rates [published online ahead of print, 2020 Jun 15]. QJM. 2020;hcaa202. doi:10.1093/qjmed/hcaa202